For much of the COVID-19 pandemic, there were few effective treatments — and no easy-to-take oral pill to treat infection with SARS-CoV-2, the coronavirus that causes COVID-19.
That changed when the Food and Drug Administration authorized Paxlovid, an antiviral pill made by Pfizer, at the end of 2021.
The drug had posted impressive results in a randomized controlled trial, which found high-risk patients who took the pills within five days of developing symptoms were nearly 90% less likely to develop severe COVID-19 than those who received a placebo. The trial, which did not include any vaccinated participants, was stopped early because the findings were so good.
But to start, supplies of Paxlovid were highly limited. Months later, the drug is becoming more widely available, but roadblocks remain in getting the treatment to those who are eligible.
 In late April, the Biden administration announced a new push to expand access, including more locations where Paxlovid is available and additional Test-to-Treat sites, or places where patients can be tested and receive and fill a prescription in one visit. The government is also conducting a public awareness campaign and communicating to providers that there is now an abundant supply of the drug.
In late April, the Biden administration announced a new push to expand access, including more locations where Paxlovid is available and additional Test-to-Treat sites, or places where patients can be tested and receive and fill a prescription in one visit. The government is also conducting a public awareness campaign and communicating to providers that there is now an abundant supply of the drug.
Meanwhile, some patients and physicians have noticed that at least on some occasions, those taking Paxlovid may get better and test negative, but then test positive again and have their symptoms return once they finish the pills — an unexpected twist during a pandemic that keeps dishing out surprises.
Given the renewed attention to the drug and the curious “rebound” phenomenon, we’ll explain what is known about Paxlovid at this time.
What is Paxlovid?
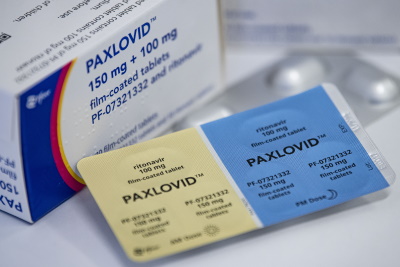
Paxlovid is the brand name of Pfizer’s oral antiviral treatment for COVID-19. It consists of two sets of pills that are taken together. The primary pill is nirmatrelvir, which is a new protease inhibitor that prevents replication of SARS-CoV-2. It’s paired with an existing drug known as ritonavir, which slows breakdown of nirmatrelvir in the liver to boost levels of that drug in the blood.
The standard course of the drug is to take two nirmatrelvir pills with one ritonavir tablet twice a day for five days, for a total of 30 pills.
As an antiviral, Paxlovid should be taken as soon as possible after someone gets sick, and is not meant for people who have already been hospitalized for COVID-19. Based on the results of a randomized controlled trial, the FDA authorized the drug for emergency use in late December 2021 for people with mild to moderate COVID-19 who are at high risk for developing severe disease. (See the section “Who is eligible to take Paxlovid?” for details on those considered high-risk.)
How effective is Paxlovid?
Paxlovid has been found to be about 88% effective in preventing hospitalization and death in unvaccinated, high-risk adults with COVID-19.
Those results come from a randomized, double-blind, placebo-controlled clinical trial published in the New England Journal of Medicine in February, which included 2,246 non-hospitalized participants with symptomatic COVID-19 who were neither vaccinated nor previously infected. All were either 60 years or older or had at least one chronic medical condition that put them at higher risk of developing severe COVID-19.
In the trial, all 13 deaths that occurred were in the placebo arm. Among the 1,039 patients who took a five-day course of Paxlovid within five days of developing symptoms, eight, or 0.8%, were hospitalized for COVID-19 or died from any cause after 28 days of follow-up. That compares with 66 of the 1,046, or 6.3%, placebo participants, which works out to an 87.8% relative risk reduction. Participants who received Paxlovid within three days of developing symptoms had an 88.9% lower risk of hospitalization or death.
The study also found that people taking Paxlovid had a viral load that was around 10 times lower than those receiving placebo, evidence that the drug does prevent replication of SARS-CoV-2 in humans.
How does Paxlovid compare with other outpatient treatments?
Paxlovid is the preferred treatment for high-risk outpatients, according to the National Institutes of Health COVID-19 treatment guidelines. Other authorized treatments exist, but are either less effective than Paxlovid or more difficult to administer.
The antiviral remdesivir, which has shown a similar level of protection against hospitalization or death when provided early, must be given intravenously over three days.
Monoclonal antibodies, which also must be given through an IV, worked well against earlier forms of the coronavirus, but have fared poorly against the omicron variant and its sub-variants. Only one monoclonal antibody, bebtelovimab, works against the BA.2 version of the omicron variant that has predominated in the U.S. since at least early April.
Molnupiravir, the only other antiviral pill, was shown in a randomized controlled trial to reduce hospitalization or death by 30% — far lower than Paxlovid’s nearly 90% reduction.
While both Paxlovid and molnupiravir prevent viral replication of the coronavirus, the two drugs work differently. Molnupiravir is a nucleoside analog that introduces errors into the virus’s genetic code, which keeps the virus from surviving and propagating. Paxlovid, in contrast, targets the virus’s protease, which shuts down viral protein processing and keeps new viruses from being made.
Does Paxlovid work in vaccinated people?
The FDA allows Paxlovid to be used in vaccinated people, but the primary trial underpinning the authorization only included high-risk people who had not been vaccinated. So it’s not known whether the drug is effective in such people.
Pfizer was conducting a study to help answer this question as part of its evaluation of Paxlovid in “standard risk” people. In that trial, the company was testing Paxlovid in unvaccinated people at low risk of hospitalization or death and also initially included vaccinated higher-risk adults with at least one risk factor for severe disease.
But in April, Pfizer expanded the trial and changed the enrollment criteria to exclude anyone with a COVID-19 vaccination in the past year. Some scientists have interpreted this move as an indication that the study was not finding much of a benefit of Paxlovid in vaccinated people.
“Based on pfizer’s actions, there seems to be minimal benefit,” Dr. David Boulware, an infectious disease specialist at the University of Minnesota, told us in an email.
Pfizer had previously announced interim results for its standard risk trial back in December, when it gave the final results for its trial of high-risk patients. Those interim results included a 70% reduction in hospitalization — which was not quite statistically significant — and a 10-fold decrease in the viral load of patients treated with Paxlovid at day five, compared with placebo. But the trial had not succeeded on its primary endpoint of alleviating symptoms with Paxlovid. The company did not report a breakdown of any results by vaccination status.
Susan S. Ellenberg, a biostatistician and clinical trial expert at the University of Pennsylvania, told us that the release of the interim results of an ongoing study is very rare.
“It’s highly unusual to report publicly interim results, and it’s certainly suspect when you make changes to the trial,” she said, although she emphasized that there may be information about the situation she doesn’t know.
Typically, interim results are only shared if a trial is stopped on the recommendation of the external data safety monitoring committee, Ellenberg said. Such committees serve as firewalls to keep companies unaware of how the treatment and placebo groups are doing.
“Once you know the interim results, the problem with that, is that if you then make changes in the study,” she said, “those changes could well be motivated by what you saw.”
When asked why the interim results were shared, Pfizer spokesperson Kit Longley said it was because the primary endpoint wasn’t met. But Ellenberg said that doesn’t make sense, since endpoints often aren’t met in the interim analysis. In those cases, unless the data suggest the trial could be futile, the data monitoring committee recommends the trial continue, since the trial could still be successful at the final analysis.
Longley told us that the protocol change was driven by ethical concerns. Once the FDA had authorized Paxlovid for all high-risk patients, regardless of vaccination, he said, it was “no longer ethical to randomize these patients into a placebo-controlled trial.” So the high-risk vaccinated group was dropped, and the trial began allowing vaccinated patients without risk factors as long as their last vaccination was at least a year ago.
“The purpose of limiting to patients whose last vaccination occurred ≥12 months prior is to enrich the study population for individuals whose immunity may be waning and who may be at elevated risk of severe COVID-19, hospitalization or death,” Longley said in an email.
Despite the uncertainty, multiple experts told us it’s likely Paxlovid has at least some benefit in vaccinated people.
“In my mind, it’s not a question of if there’s benefit in people who are vaccinated,” University of Pennsylvania infectious disease fellow Dr. Aaron Richterman said, given the mechanism of the drug and the “strong evidence” in people at highest risk. “The question is really going to be, what amount of benefit is there going to be?”
Globally, he said, the people who should really get the drug are people who are unvaccinated and high-risk. But just considering an individual patient before him, Richterman said the likelihood of Paxlovid helping a vaccinated person is high, even if the benefit might be small.
Boulware, who suspects the benefit is minimal, said that minimal is still “greater than no benefit.” He added, “If people are immunocompromised, then absolutely there is a benefit or if they have high risk comorbidities.”
Other experts also told STAT that the lack of data in vaccinated people does not make them feel uncomfortable prescribing the drug for high-risk vaccinated people.
Some answers may come when the full results of the Pfizer trial are released, which Longley said would likely be in the second half of the year. Or, they may come from the University of Oxford’s PANORAMIC trial, which recently added Paxlovid to the study and is open to participants regardless of vaccination status.
What is known about the relapses some patients seem to have after taking Paxlovid?
Some patients who have taken Paxlovid have reported recovering and testing negative, but then falling ill and testing positive again on an antigen test a few days after completing their treatment.
In most cases, patients don’t seem to be very sick, but some report having worse symptoms than before. Since there are only anecdotal reports of this phenomenon, it’s unclear how frequently this occurs, how concerning it is, and whether it’s necessarily due to the use of the pills.
Pfizer has argued that data from their clinical trial suggests that such viral rebound is not specific to those receiving Paxlovid. In an email to FactCheck.org, Longley, the Pfizer spokesperson, said that “a small number of participants” in both arms of its trial of high-risk patients had higher viral loads 10 to 14 days after starting treatment compared with day five — and there was no link between a viral load increase and subsequent severe disease. “Although it is too early to determine the cause, this suggests the observed increase in viral load is both uncommon and not uniquely associated with treatment,” he wrote.
Pfizer similarly told NBC News that in the trial, about 2% of participants who received Paxlovid experienced rebound, while 1.5% of those on placebo did.
Dr. Paul E. Sax, the clinical director of infectious diseases at Brigham and Women’s Hospital who has been following the issue on his New England Journal of Medicine blog, noticed that some viral rebound has been documented before. The FDA’s review of Paxlovid noted that “several” subjects appeared to have a rebound around day 10 or 14, but that there was no evidence it was associated with antiviral resistance.
The FDA directed us to a Q&A for providers posted on its website, which said that the agency has performed additional analyses of the Paxlovid clinical trial data following reports of relapse.
“In the Paxlovid clinical trial, some patients (range 1-2%) had one or more positive SARS-CoV-2 PCR tests after testing negative, or an increase in the amount of SARS-CoV-2 detected by PCR, after completing their treatment course,” Dr. John Farley, director of the FDA’s Office of Infectious Diseases, wrote. “This finding was observed in patients treated with the drug as well as patients who received placebo, so it is unclear at this point that this is related to drug treatment. Additional analyses show that most of the patients did not have symptoms at the time of a positive PCR test after testing negative, and, most importantly, there was no increased occurrence of hospitalization or death or development of drug resistance.”
But many clinicians are convinced that the phenomenon, which includes a relapse of symptoms, is related to Paxlovid use.
“It’s real, but also pretty rare,” Boulware said.
Richterman, the Penn infectious disease fellow, agreed. “Most ID docs who are seeing this, myself included, suspect that there’s a real phenomenon going on,” he said, although he added that there remains a lot of uncertainty.
He said that it’s true that a small percentage of people experience an uptick in their viral loads later in their infections. Data from a study of professional basketball players in the NBA, which includes individual viral load curves, shows that, Richterman said. But those viral loads usually haven’t returned to a very high level.
“In the anecdotes that we’ve seen here, the people become very positive again with very high viral loads and are symptomatic. And so, it seems that this process is different,” he said, cautioning that the phenomenon hasn’t been well characterized yet.
The most complete understanding of a single case comes from an unpublished case report from researchers in Boston, who describe a relapse in a 71-year-old vaccinated and boosted man. His symptoms resolved soon after taking Paxlovid, but a week later he developed cold-like symptoms, and his viral load rebounded with his illness. Sequencing from viral samples from the man suggest that he was not reinfected, nor was there any sign that the virus had mutated to get around Paxlovid treatment. The authors propose that very early treatment with Paxlovid might temporarily reduce the amount of virus in the body before the immune system has a chance to fully clear the pathogen.
Indeed, several scientists think what could be happening is that Paxlovid treatment could stunt or delay the immune response. It’s also possible relapse is occurring in certain people because of idiosyncrasies of their immune systems, University of North Carolina at Chapel Hill virologist Timothy Sheahan told us.
“All [Paxlovid] is doing is stopping viral protein processing, stopping the protein from making new viruses,” he said. “But those particular cells that are infected are still infected and there’s still viral RNA there. So if you take the drug away, that could continue [replication] in those cells if they don’t die.”
But no one knows for sure, and multiple things could be happening, too, he said.
Scientists agree it will be important to investigate the rebounds to find out why they are occurring, if certain people are at higher risk for them, whether such individuals are contagious during them, and what the best clinical approach is for handling them.
One big concern is that these cases could be breeding grounds for Paxlovid drug resistance. “Resistance is definitely something that should be on everybody’s radar,” said Sheahan. “Whenever you have incomplete success in your treatment, it’s an opportunity for the generation of resistance.”
Sheahan, who has studied coronavirus antivirals, said it will be important to sequence viruses from those experiencing rebounds and see whether there are changes in the protease that Paxlovid targets. “This needs to be followed up in a very methodical and rigorous way to understand how the virus may be changing,” he said.
Some of those experiments have been done, and there is no evidence that that is occurring yet. But with more people taking the drug, the opportunity for resistance increases, Sheahan said. A longer course of the drug could do the trick, if that’s enough to stop the rebounds, or Paxlovid could be paired with another medicine in a cocktail to greatly lower the odds of creating drug-resistant viruses, he said.
In a statement to FactCheck.org, the NIH said that in collaboration with the Centers for Disease Control and Prevention and the FDA, it was “looking into possible ways to better understand” the rebounds, and that while it does not have studies already underway, “the agency is actively discussing potential studies to learn more about who this is affecting, how often it is occurring and if a longer regimen would be more effective in certain cases.”
What should you do if you have a relapse on Paxlovid?
Clinicians are still learning about the relapses, so there isn’t firm advice yet. But most doctors say that if you have symptoms and test positive again, then you should assume you are contagious and isolate to prevent spreading the virus to others.
When asked whether individuals experiencing rebound should extend their isolation, a CDC spokesperson said that “anyone who develops symptoms of illness during or after isolation should remain isolated, masked, and seek out testing and clinical care.”
Update, May 27: The CDC said in a May 24 health alert that people who have a recurrence of symptoms or test positive again should “restart isolation and isolate again for at least 5 days.” It also said that there is “currently no evidence that additional treatment for COVID-19 is needed for COVID-19 rebound.”
There is also debate — and confusion — about whether physicians should or are allowed to give patients, many of whom could be quite vulnerable, more Paxlovid if they relapse. Pfizer’s CEO recommended doing so in a May 3 interview with Bloomberg News.
But without commenting directly, the FDA has suggested that giving more than five days of the drug in a rebound situation is not permitted under the emergency use authorization. (If the drug were fully approved, it would be allowed.)
“Health care providers should consider treatment with Paxlovid or other approved or authorized therapeutics in accordance with the approved labeling or authorized Health Care Provider Fact Sheets,” FDA’s Farley wrote in his Q&A on Paxlovid, adding that there is “no evidence of benefit at this time for a longer course of treatment (e.g., 10 days rather than the 5 days recommended in the Provider Fact Sheet for Paxlovid) or repeating a treatment course of Paxlovid in patients with recurrent COVID-19 symptoms following completion of a treatment course.”
Pfizer has since told us that it agrees with the FDA on this, but said that there are “no limitations within the authorized label around use for subsequent COVID-19 infections.” Subsequent infections, however, are different from the relapse phenomenon as it is understood now.
Richterman, for example, was under the impression that the FDA would allow another course of Paxlovid — and said he thought it would be reasonable for some people if their symptoms were bad enough, even though there isn’t good data to support that approach. But for vaccinated and boosted people with mild symptoms, he said, it would also be reasonable to wait it out a couple of days.
How safe is Paxlovid?
From the clinical trials, Paxlovid appears to be quite safe, although this will continue to be studied and monitored. In the main trial of high-risk COVID-19 patients in which patients took the drug for five days, there were no major safety concerns. Possible side effects include a temporary altered sense of taste, diarrhea and vomiting, along with muscle aches and high blood pressure.
Paxlovid, however, does pose risks to some with liver and kidney disease and interacts with a large number of drugs, so certain people should not take it, or may need to take a different Paxlovid dose or temporarily stop taking their normal medications, including some common cholesterol-lowering drugs.
Much of that is due to the ritonavir component of Paxlovid, which inhibits an enzyme in the liver that breaks down many medicines. While blocking the enzyme is necessary to increase the levels of the protease part of Paxlovid, it can cause problems for patients taking other drugs, as the FDA explained in announcing the authorization.
For patients with kidney disease, those with moderate renal impairment should take a lower dose of Paxlovid that comes in a separate dose pack, while those with mild impairment can take the normal dosage and those with severe impairment should not take it at all.
Who is eligible to take Paxlovid?
Paxlovid is authorized for adults and kids 12 years of age and older who weigh at least 88 pounds. To be eligible for a prescription, you must have tested positive for SARS-CoV-2 infection, have mild to moderate disease, and be at high risk of becoming severely ill. You must also have had symptoms for no longer than five days.
“High risk” means being 65 years — or even 50 years — and older or having at least one medical condition listed on the CDC website that increases a person’s COVID-19 risk, such as obesity or being overweight, diabetes, and heart or lung diseases.
The CDC list isn’t exhaustive, though, so you’re not necessarily disqualified if you don’t have one of the listed conditions. Being vaccinated does not make you ineligible, but not being vaccinated or boosted could be considered a risk factor, according to the FDA.
To receive Paxlovid you need a prescription from a health care provider, who will assess whether you are high risk and whether the drug is right for you.
Does Paxlovid work as a preventive?
No, Paxlovid does not appear to be able to prevent infection, at least the way it has been tested so far. In late April, Pfizer shared results from its post-exposure prophylaxis trial, which failed to demonstrate that Paxlovid could protect adults from getting a symptomatic infection from someone in their household with COVID-19.
The study included nearly 3,000 participants who were randomly assigned to take a placebo or a five- or 10-day course of Paxlovid within 96 hours of exposure to a recently infected household contact. According to Pfizer, those who received a five- and 10-day course of the drug were 32% and 37% less likely, respectively, to develop a symptomatic infection compared with placebo. But the results were not statistically significant, and could have occurred by chance.
This failure could be due to a variety of reasons. The drug might simply be incapable of preventing infection because of the way it works, interfering late in the process of viral replication, for example. Or, the trial may not have started its participants on Paxlovid early enough. Regardless, as multiple experts told STAT, the negative results don’t change the utility of the drug as a treatment.
Editor’s note: SciCheck’s COVID-19/Vaccination Project is made possible by a grant from the Robert Wood Johnson Foundation. The foundation has no control over FactCheck.org’s editorial decisions, and the views expressed in our articles do not necessarily reflect the views of the foundation. The goal of the project is to increase exposure to accurate information about COVID-19 and vaccines, while decreasing the impact of misinformation.